INTRODUCTION
Pregnancy-associated neurocritical complications involve various diseases. Myasthenia gravis can be worsened in approximately 30% to 40% of women during pregnancy or during the postpartum period [1]. The relapse rate of multiple sclerosis increases in the 3 months postpartum [2]. Approximately one-third of pregnant women with epilepsy can experience worsening of seizure control due to various factors such as psychological stress, sleep deprivation, altered drug disposition, poor drug compliance due to fear of teratogenicity, increased estrogen levels leading to decline in seizure threshold, and decreased serum levels of antiepileptic drugs [3-5]. Pregnancy-related cerebrovascular disorder is one of the major causes of maternal mortality. In the present review, we focus especially on cerebrovascular complications during pregnancy and postpartum. These complications are closely related to physiological changes during pregnancy. Thus, it is important to understand the changes in the hemodynamic, vascular structural, and coagulation systems that can occur during pregnancy.
WHAT HAPPENS DURING PREGNANCY?
Cardiac output and blood volume increase 30% to 50% until late in the second trimester due to maternal hypervolemia and the developing fetus [6-8]. However, increased nitric oxide and prostacyclin levels cause systemic vascular resistance to begin to lower blood pressure [9]. In addition, increased venous capacitance compromises venous stasis, which leads to orthostatic intolerance [10,11]. Concurrently, the collagen and elastin content of systemic arteries decrease [10,12]. More vulnerable vessel walls encounter greater hemodynamic stress. Both hemodynamic and structural changes in vessel walls during pregnancy can contribute to the increased risk for various hemorrhagic conditions in the brain.
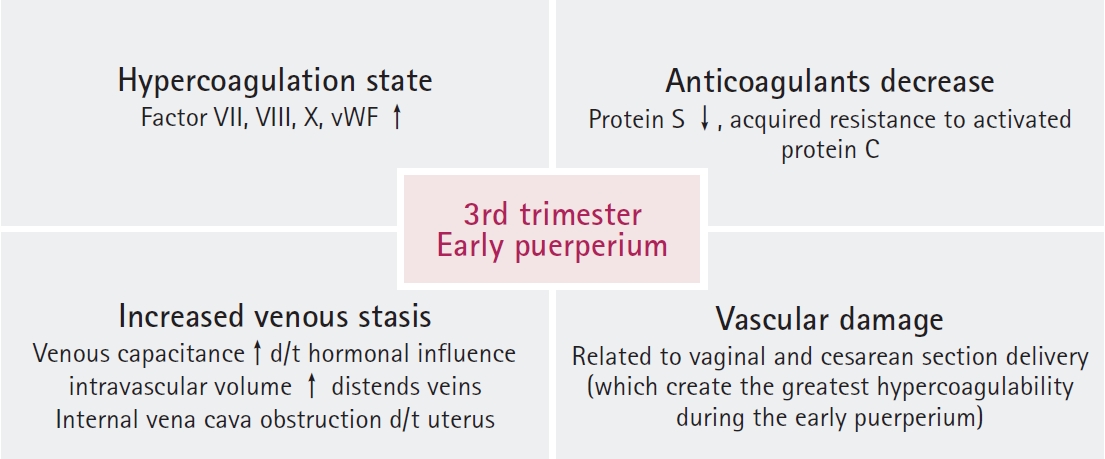
In the third trimester of pregnancy and the early puerperium period, venous congestion, aortocaval compression by gravid uterus, and vascular damage related to vaginal or cesarean section delivery can induce hypercoagulability [13-15]. Biochemical changes, such as increased procoagulants (Factors VII, VIII, and X) and decreased coagulation inhibitors (antithrombin III and protein S) in late pregnancy, also result in a hypercoagulable state (Fig. 1) [15-17].
RISK FACTORS FOR THROMBOEMBOLISM DURING PREGNANCY AND POSTPARTUM
The strongest risk factors for venous thromboembolism (VTE) is a history of thrombosis, and pregnancy-related hypertension for both ischemic and hemorrhagic stroke during pregnancy and puerperium [16,17]. According to population-based studies, advanced maternal age (>35 years), obesity (body mass index >30 kg/m2), multiple births, and multiple gestation are characteristics that can increase the risk for thromboembolism [16,18]. In terms of medical conditions and pregnancy complications, heart disease, systemic lupus erythematosus, immobilization, smoking, inflammatory bowel disease, cesarean delivery, preterm delivery (<36 weeks), transfusion, preeclampsia and eclampsia can amplify the maternal thromboembolic risk [16,19,20]. The inherited thrombophilias associated with thromboembolism in pregnancy is a genetic tendency of VTE in particular. Factor V Leiden mutation and prothrombin 20210A mutation are more common inherited thrombophilias in Caucasian populations [21]. However, Kim et al. [22] reported that a Factor V Leiden mutation and a prothrombin 20210A mutation was not found in 228 Korean patients with VTE. Another study also reported no Factor V Leiden mutation in Korean patients with deep vein thrombosis (DVT). As such, these inherited thrombophilias appear to be extremely rare in Asian populations, including Koreans with DVT [23]. On the other hand, deficiencies in antithrombin, protein S and protein C, and antiphospholipid syndrome, are relatively common in Korean populations, and are stronger risk factors [22,24-27].
Pregnancy-related hypertensive disorder is one of the leading causes of neurocritical illness in the perinatal or postnatal periods [28,29]. In particular, preeclampsia, eclampsia and HELLP syndrome (hemolysis with a microangiopathic blood smear, elevated liver enzymes and low platelets) represent the most important spectrum of pregnancy-related hypertensive disorders in the latter half of pregnancy or postpartum, which lead to increased risk for thromboembolic and hemorrhagic complications [28]. In 2019, the American College of Obstetricians and Gynecologists listed diagnostic criteria for preeclampsia (Table 1) [30]. Eclampsia (convulsive manifestation of preeclampsia) and HELLP syndrome are more severe forms of preeclampsia [30].
VENOUS THROMBOEMBOLIC COMPLICATIONS DURING PREGNANCY AND POSTPARTUM
Thromboembolism in pregnancy occurs in approximately 0.5 to 2.0 per 1,000 deliveries [15,31,32]. The risk for developing thromboembolism increases by a factor of 4 to 5 during pregnancy, and by up to 20 to 80 during the 3 months following delivery [33]. In particular, 2 weeks after delivery is the most critical period [34], accounting for approximately 10% of maternal mortality, resulting in 1.1 to 1.5 deaths per 10,000 deliveries [16].
Of pregnancy-related thromboembolisms, approximately 80% occur in the venous system, of which arterial thromboembolism accounts for 20% [35]. There are various mechanisms of VTE. The most common complication of VTE is DVT, which occurs in 80% of patients with VTE. Pulmonary thromboembolism (PTE) is the second most common cause [35]. It is difficult to diagnose DVT or PTE in pregnant women because approximately 50% of patients exhibit no specific symptoms, and common lower extremity symptoms in DVT, or tachycardia, tachypnea or dyspnea in PTE can occur in women who are pregnant.
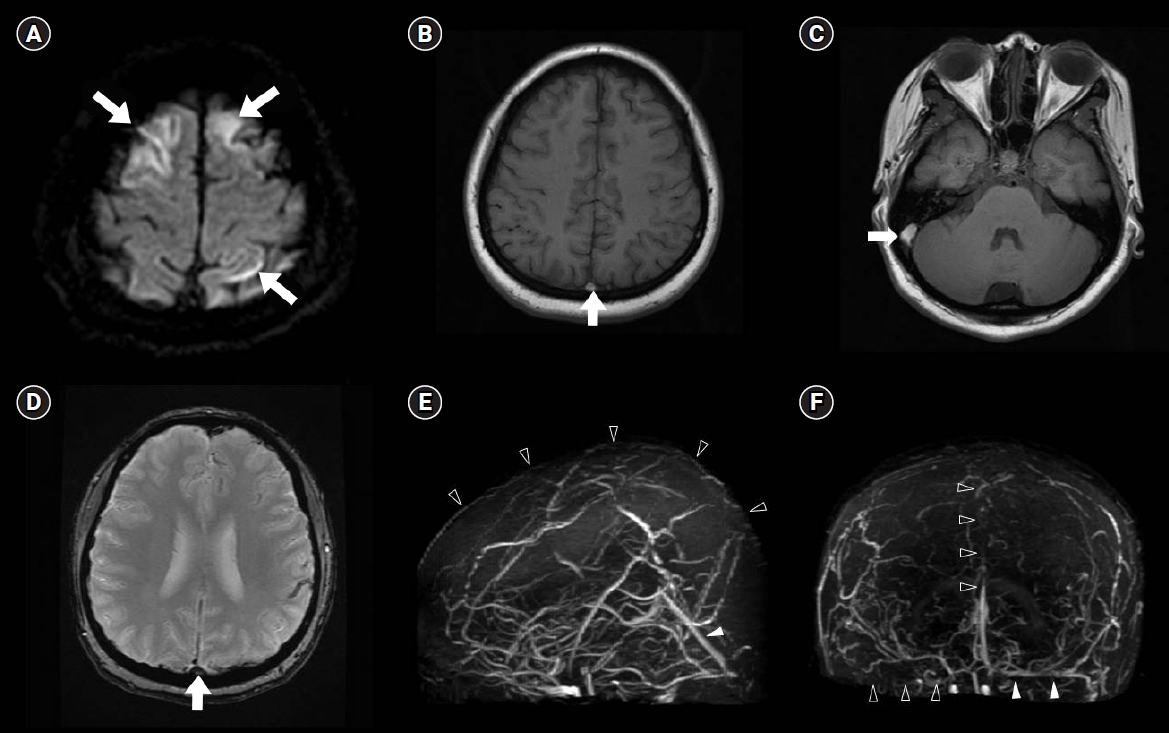
Cerebral venous thrombosis (CVT) accounts for 2% to 37% of pregnancy-associated strokes [36,37]. Clinical presentations of CVT are characterized by headache, papilledema, visual loss, motor deficits, seizures, focal neurological deficits, and altered mentality depending on the involved cerebral vein and sinus (Fig. 2) [34,38]. Compared with CVT unrelated to pregnancy and puerperium, pregnancy-related CVT has an acute onset with a progressive course and, more often, concomitant extraneurological thromboembolism. Nevertheless, CVT during pregnancy and puerperium can be diagnosed earlier and its symptoms tend to subside or become stable faster, thereby resulting in better outcomes with lower mortality [34].
TREATMENT OF VTE DURING PREGNANCY AND POSTPARTUM
Treatment of VTE during pregnancy is highly unique in many ways. Warfarin is a commonly used anticoagulant able to cross the placenta and may be teratogenic in the first trimester. In the third trimester, warfarin can increase the risk for bleeding in fetal intracranial bleeding [39,40]. Thus, its use during pregnancy should be avoided [41]. Direct oral anticoagulants are not recommended during pregnancy because their efficacy and safety have not been established, and should also not be used in women who are breastfeeding during puerperium [42]. The treatment of choice for VTE in pregnant women is subcutaneously administered low-molecular weight heparin (LMWH), which does not cross the placental barrier [43,44]. There is no fetal risk for bleeding or teratogenicity. Although intravenous (IV) unfractionated heparin can be considered as an alternative, subcutaneous LMWH is preferred over IV unfractionated heparin due to its higher bioavailability and a longer plasma half-life. Additionally, the use of LMWH is easier and appears to be more efficacious, with fewer bleeding complications [16,41].
The proportion of patients who present with intracranial hemorrhages, such as venous hemorrhage, hemorrhagic infarction or, rarely, subarachnoid hemorrhage (SAH), represent approximately one-third of patients with CVT [45]. The presence of intracranial hemorrhage, however, is not a contraindication to anticoagulants in the management of CVT.
Reasonable initial dosing of subcutaneous LMWH is 1 mg/kg of enoxaparin every 12 hours, 100 units/kg of dalteparin every 12 hours, or 200 units/kg of dalteparin once daily. LMWH should be discontinued 24 hours before induction of labor or cesarean section and resumed 4 to 6 hours after vaginal delivery, or 6 to 12 hours after cesarean delivery [46]. Treatment should be continued for at least 6 weeks after delivery. Although warfarin metabolites are detected in breast milk, their low activity makes it safe to use warfarin during lactation [47]. There are also no contraindications to breastfeeding while undergoing unfractionated heparin or LMWH therapy.
ARTERIAL THROMBOEMBOLIC COMPLICATIONS DURING PREGNANCY AND POSTPARTUM
Arterial thromboembolism is a less common complication but is, however, more critical and disabling. The incidence of pregnancy-associated stroke is 25 to 34 per 100,000 deliveries, a figure that has been rising steadily [36,48]. In comparison, the incidence of stroke unrelated to pregnancy in women 15 to 45 years of age is approximately 11 per 100,000 deliveries [49].
The risk for arterial ischemic stroke is higher during puerperium than during pregnancy. A previous study by Kittner et al. [50] reported that the risk for ischemic stroke increased in the puerperium period but not during pregnancy. Hemorrhagic stroke occurred more frequently during the second or early third trimesters, and in the early postpartum period. More specifically, the risk for aneurysmal SAH peaks at 30 to 34 weeks of pregnancy; however, intracerebral hemorrhage occurs more during puerperium than in pregnancy [50]. Approximately 50% of all aneurysmal ruptures in women <40 years of age are pregnancy-related. Arteriovenous malformations (AVMs), however, are more controversial. One study reported that cerebral hemorrhage due to AVMs associated with pregnancy occurred evenly throughout the entire gestation and postpartum periods [51,52].
Although there are many causes of stroke during pregnancy or puerperium, most are similar, with common etiologies such as ischemic or hemorrhagic stroke; however, pregnancy-specific causes include preeclampsia/eclampsia. Amniotic fluid embolism, AVMs, cerebral artery aneurysm, posterior reversible encephalopathy syndrome (PRES), and postpartum angiopathy (PPA) are also well-known causes [53-56].
PRES AND PPA DURING PREGNANCY AND POSTPARTUM
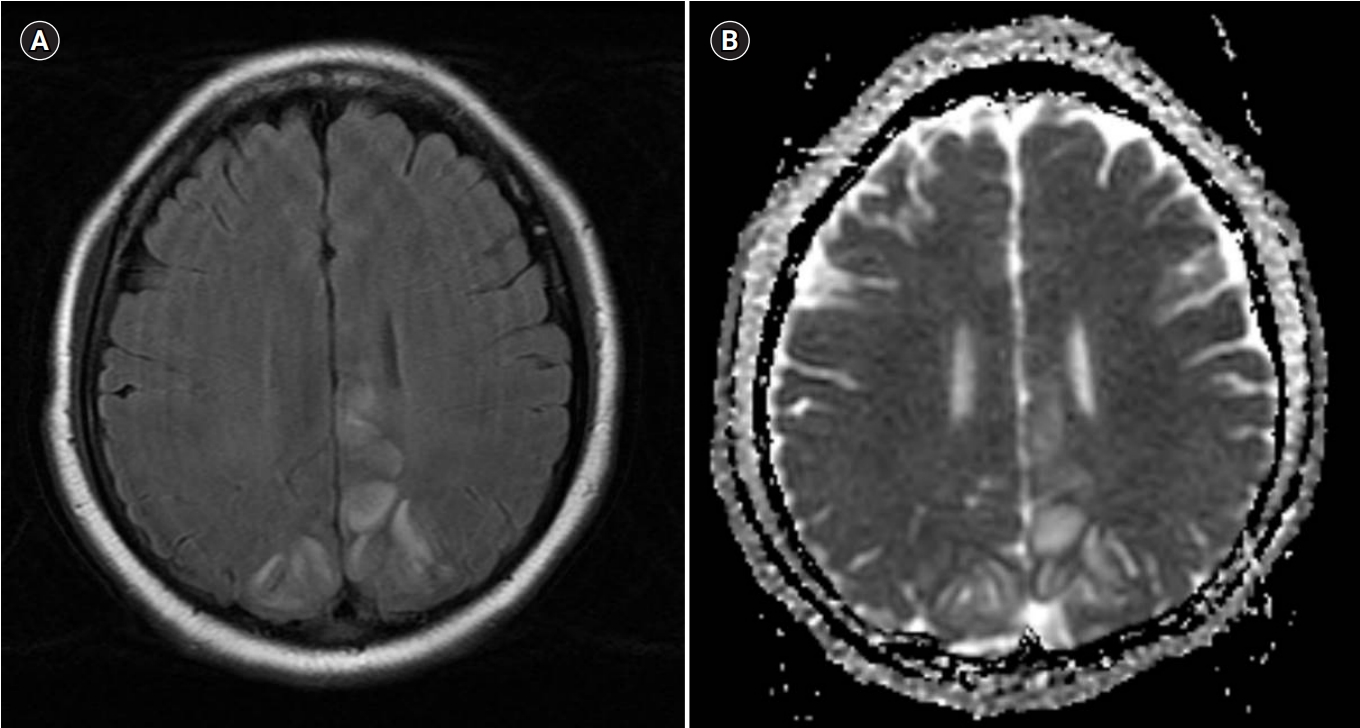
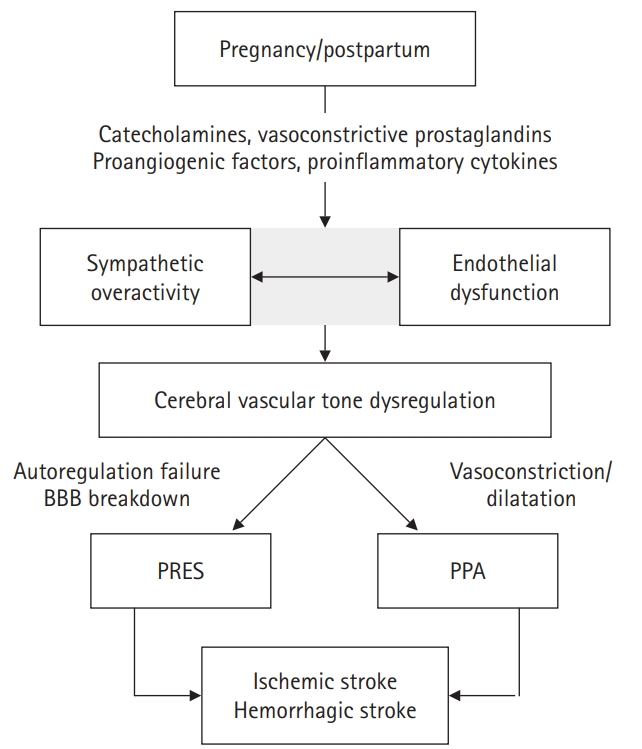
PRES is a clinical and radiographic syndrome and is classically characterized by vasogenic edema in the bilateral parietooccipital lobes (Fig. 3). Symmetrical hyperintense signals on T2 and fluid-attenuated inversion recovery magnetic resonance imaging, with increased value on the apparent diffusion coefficient map, can also be evident in atypical areas such as the basal ganglia, frontal lobes, cerebellum, and brainstem [57,58]. Approximately 20% of CVT can be accompanied by hemorrhagic stroke [53,59]. The mechanism is not completely understood; however, a breakdown of the blood-brain barrier and cerebral auto-regulation attributed to hyperperfusion results in extravasation of fluid containing blood by-products into the brain parenchyma, which in turn causes vasogenic edema. Endothelial dysfunction also plays a key role in the mechanism, and is especially associated with preeclampsia (Fig. 4). The levels of serological markers of endothelial dysfunction are increased during pregnancy with preeclampsia [60,61]. With regard to anatomical distribution, sympathetic innervation in the posterior circulation is relatively scant compared with the anterior circulation [62]. Sympathetic innervation of the intracranial arterioles has a protective role in rapid and dynamic fluctuations in blood flow. The posterior circulation, therefore, is vulnerable to breakthrough of the blood-brain barrier and failure of cerebral autoregulation.
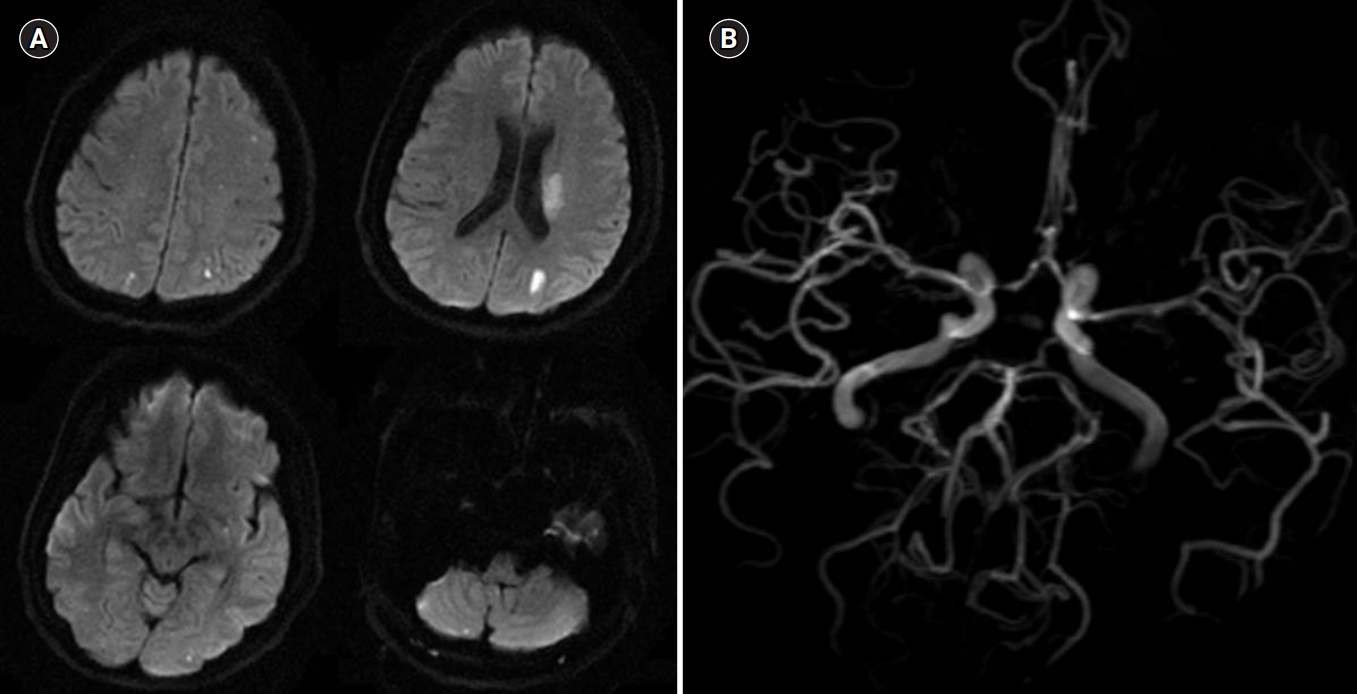
PPA, one of the spectrums of reversible cerebral vasoconstriction syndrome, is a noninflammatory vasoconstrictive condition [63]. Two-thirds of PPA cases occur in the first week after delivery [64]. Patients with PPA exhibit reversible segmental constrictions and dilatations of large- or medium-size cerebral arteries (Fig. 5), and approximately 40% of PPA can be accompanied by intracranial hemorrhage [54]. PPA and PRES share many clinic-radiological features and pathophysiological mechanisms, and are considered to be overlapping conditions (Fig. 4) [65,66]. More than 85% of PRES exhibits multifocal vasoconstriction of the cerebral arteries and reversible cerebral edema occurs in approximately one-third of PPA cases. Both can present with thunderclap headache, seizure, and focal neurological deficits such as visual symptoms. Usually, however, they have a self-limited benign course, and radiological abnormalities are resolved within several days to weeks [67]. Steroid is not a recommended therapy for pregnancy-associated PRES [48,63]. Although there is no supportive therapeutic evidence, short-term steroids, oral calcium channel blockers, and/or IV magnesium are administrated by some physicians for PPA [54]. As such, it remains controversial whether these treatments are effective in altering the natural disease course. However, 10% can be exacerbated by severe vasoconstriction and cerebral edema, leading to fulminant neurological deficits or death.
TREATMENT OF STROKE DURING PREGNANCY AND POSTPARTUM
The treatment of stroke during pregnancy and postpartum is guided by etiology and subtype. The safety of reperfusion strategies for pregnant women who experience acute ischemic stroke remains uncertain. IV alteplase does not cross the placenta because of its large molecular weight, but is listed as a pregnancy category C drug [68]. The major concern for administration of IV alteplase is the risk for maternal and fetal bleeding. Previous stroke guidelines have listed pregnancy as a relative exclusion criterion [69]. A recent study using the American Heart Association’s Get With the Guidelines-Stroke Registry showed that 40 pregnant or postpartum women receiving emergent reperfusion therapy for acute ischemia exhibited a trend toward increased symptomatic intracranial hemorrhage compared with nonpregnant young women undergoing reperfusion therapy. However, they had more severe stroke severity, which is one of the major risk factors for symptomatic intracranial hemorrhage. Nevertheless, there were no significant differences in functional outcomes at discharge, life-threatening hemorrhage, and in-hospital mortality between pregnant or postpartum and nonpregnant women with ischemic stroke who received reperfusion therapy [70]. The updated 2018 American Heart Association/American Stroke Association guidelines reported that IV alteplase administration may be considered in the management of acute ischemic stroke for pregnant women when the anticipated benefit of IV alteplase outweighs the potential risk(s) for bleeding [71]. Recently, direct endovascular thrombectomy without IV alteplase has been attempted as an alternative treatment for pregnant women with a potentially high risk for bleeding on IV alteplase.
For antiplatelet therapy, the administration of aspirin can be considered in patients who experience acute ischemic stroke and have contraindications to anticoagulants [72]. Although ischemic stroke occurs less frequently during the first trimester of pregnancy, data regarding the safety of daily aspirin use during this period are limited. Aspirin can cross the placenta and increase the risk for birth defects. Therefore, daily use of aspirin is not recommended during the first trimester of pregnancy. In terms of the dose issue, high-dose aspirin is not recommended due to the risk for congenital malformation and bleeding in the brains of premature infants [72]. Previous studies using low-dose aspirin in the second and third trimester; however, demonstrated no differences in congenital defects, developmental delay, or bleeding problems [73,74]. Based on this evidence, low-dose aspirin (60 to 150 mg/day) can be used for ischemic stroke during the second and third trimesters of pregnancy [72]. There is a lack of evidence supporting the daily use of other antiplatelet medications, including clopidogrel (pregnancy category B) and dipyridamole (pregnancy category D) during pregnancy. Antithrombotic drugs should be discontinued before a planned delivery. Specific days depend on type: aspirin should be stopped 7 days before delivery, and LMWH should be discontinued 24 hours before delivery.
Early surgical clipping or endovascular coiling leads to better outcomes in pregnant women with SAH due to ruptured aneurysms [7,75]. Vaginal delivery can be safe after successful aneurysm obliteration. AVMs in pregnant women are also managed as they would in non-pregnant women. If an AVM bleeds during pregnancy, treatment depending on grade should be considered during the pregnancy [7]. Pregnant women should be always protected with shielding of the abdomen during radiological procedures and evaluations.
BLOOD PRESSURE MANAGEMENT DURING PREGNANCY
The National Institute for Health and Clinical Excellence recommends that management of hypertensive disorders during pregnancy should be initiated at blood pressures ≥150/100 mm Hg, and should be also used to maintain systolic blood pressure <150 mm Hg and diastolic blood pressure of 80 to 100 mm Hg [76]. However, all antihypertensive drugs can cross the placenta, and there are no comparative data regarding efficacy and fetal safety from large randomized trials. Labetalol, nifedipine, and methyldopa are recommended as primary options, and angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, renin inhibitor, and mineralocorticoid receptor antagonist should be avoided due to increased risk for fetopathy [77]. If IV administration is required in the acute period of severe hypertension or pregnancy-related hemorrhagic stroke, hydralazine, labetalol, or nicardipine can be used primarily. Hydralazine (5 mg IV administration for 1 to 2 minutes) is a drug widely used in the acute stage of severe preeclampsia and, if the reduction in blood pressure is insufficient, 5 to 10 mg IV administration can be further injected further up to 30 mg, with the drug effect lasting 2 to 4 hours. The initial dose of IV labetalol is 20 mg, and 20 to 80 mg IV can be administrated repeatedly every 30 minutes up to 300 mg in total. Blood pressure drops within 5 to 10 minutes and lasts 3 to 6 hours. Nicardipine can be administered intravenously in emergency cases. If the initial dose of 5 mg/hr is not effective, it can be increased to a maximum of 15 mg/hr [78].
OTHER NEUROCRITICAL CARE DURING PREGNANCY
In pregnant women with increased intracranial pressure due to various neurological complications, hypertonic saline is preferred over mannitol for osmotherapy. Mannitol can lead to fetal hypoxia and acid-base imbalances [17]. In terms of eclamptic seizure management, IV magnesium sulfate has been shown to be superior to commonly used anticonvulsants [79]. Typical dosing is 4 to 6 g over a period of 20 to 30 minutes, followed by continuous infusion of 2 g/hr. If seizures occur during treatment, additional 2 g boluses of IV magnesium sulfate may be administered.
CONCLUSION
Cerebrovascular complications during pregnancy and puerperium such as CVT, ischemic and hemorrhagic stroke, PRES and postpartum angiopathy present a challenge to neurointensivists because pregnancy is a very unique condition. Neurointensivists should understand the maternal changes in the hemodynamic, vascular structural, and coagulation systems that can occur during pregnancy and postpartum and also consider potential risk on the fetus. Knowledge of pregnancy-related cerebrovascular complications will provide optimal management for both fetus and mother.